Introduction: Shedding Light on Diabetic Nephropathy
Diabetes, a condition marked by persistently high blood sugar levels, has emerged as a significant global health issue impacting millions of people. While it is frequently linked to complications such as heart disease, vision impairment, and nerve damage, its effects on kidney health are equally critical. Among these complications, diabetic nephropathy, also known as diabetic kidney disease, is a prominent cause of kidney failure around the world.
The kidneys, essential organs that filter waste and maintain fluid balance in the body, can experience severe damage due to long-term exposure to high blood sugar and elevated blood pressure. For those living with diabetes, this damage can gradually worsen over time, often remaining unnoticed until kidney function is severely affected.
Grasping the concept of diabetic nephropathy is vital—not just for individuals with diabetes but also for their caregivers and healthcare professionals. Increased awareness and prompt intervention can help prevent or slow its progression, enhancing quality of life and lowering the risk of kidney failure.
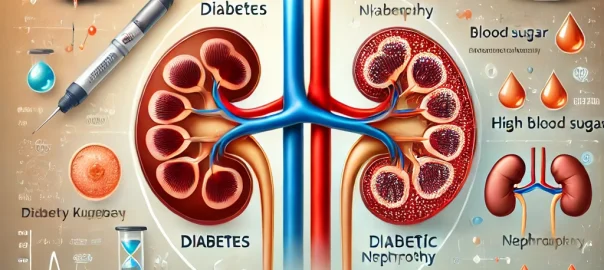
What is diabetic Nephropathy?
Diabetic nephropathy, often referred to as diabetic kidney disease, is a serious complication that arises from diabetes and affects the kidneys. It happens when consistently high blood sugar levels cause damage to the small blood vessels (glomeruli) in the kidneys, which hinders their ability to filter out waste, toxins, and excess fluids from the bloodstream. If this damage continues over time, it can result in chronic kidney disease (CKD) and, in severe instances, kidney failure, which may necessitate dialysis or a kidney transplant.
complication that arises from diabetes and affects the kidneys. It happens when consistently high blood sugar levels cause damage to the small blood vessels (glomeruli) in the kidneys, which hinders their ability to filter out waste, toxins, and excess fluids from the bloodstream. If this damage continues over time, it can result in chronic kidney disease (CKD) and, in severe instances, kidney failure, which may necessitate dialysis or a kidney transplant.
This condition is among the leading causes of kidney failure globally and has a profound effect on the lives of those with diabetes. Nevertheless, with appropriate management, its progression can often be slowed or even halted.
Key Stages of Kidney Damage in Diabetic Patients
Diabetic nephropathy progresses through distinct stages, each characterized by increasing levels of kidney damage:
Stage 1: Hyperfiltration
Initially, the kidneys work harder, filtering blood at an unusually high rate.
Early damage to the glomeruli begins, but there are typically no noticeable symptoms.
Stage 2: Microalbuminuria
Small amounts of albumin start to appear in the urine.
This stage may still be asymptomatic, but it indicates the onset of kidney damage.
Stage 3: Macroalbuminuria (Overt Nephropathy)
Protein levels in the urine rise significantly.
Patients may experience symptoms such as swelling (edema) in the legs and elevated blood pressure.
Stage 4: Chronic Kidney Disease (CKD)
Kidney function declines noticeably, leading to the accumulation of waste products in the blood.
Symptoms like fatigue, nausea, and itching may start to appear.
Stage 5: Kidney Failure (End-Stage Renal Disease, ESRD)
The kidneys lose nearly all their function.
Patients require dialysis or a kidney transplant to survive.
Diabetic nephropathy is a serious condition, but catching it early and managing it proactively can lead to significant improvements. Consistent monitoring, controlling blood sugar levels, and making lifestyle changes are essential for safeguarding kidney health and preventing the condition from advancing to its more severe stages.
Causes and Risk Factors of Diabetic Nephropathy
Diabetic nephropathy is a frequent complication of diabetes, resulting from a complex mix of factors that gradually harm the kidneys. Recognizing these causes and risk factors is vital for preventing or slowing the advancement of this condition.
1).The Role of High Blood Sugar and Hypertension in Kidney Damage
The primary factors contributing to diabetic nephropathy are persistently high blood sugar levels and uncontrolled hypertension.
High Blood Sugar (Hyperglycemia):
When blood sugar levels stay elevated for a long time, the excess glucose can harm the fragile blood vessels (glomeruli) in the kidneys. These vessels are essential for filtering waste from the blood. Over time, this damage reduces the kidneys’ ability to filter effectively, leading to protein leakage (albuminuria) and further harm to the tissue.
Hypertension (High Blood Pressure):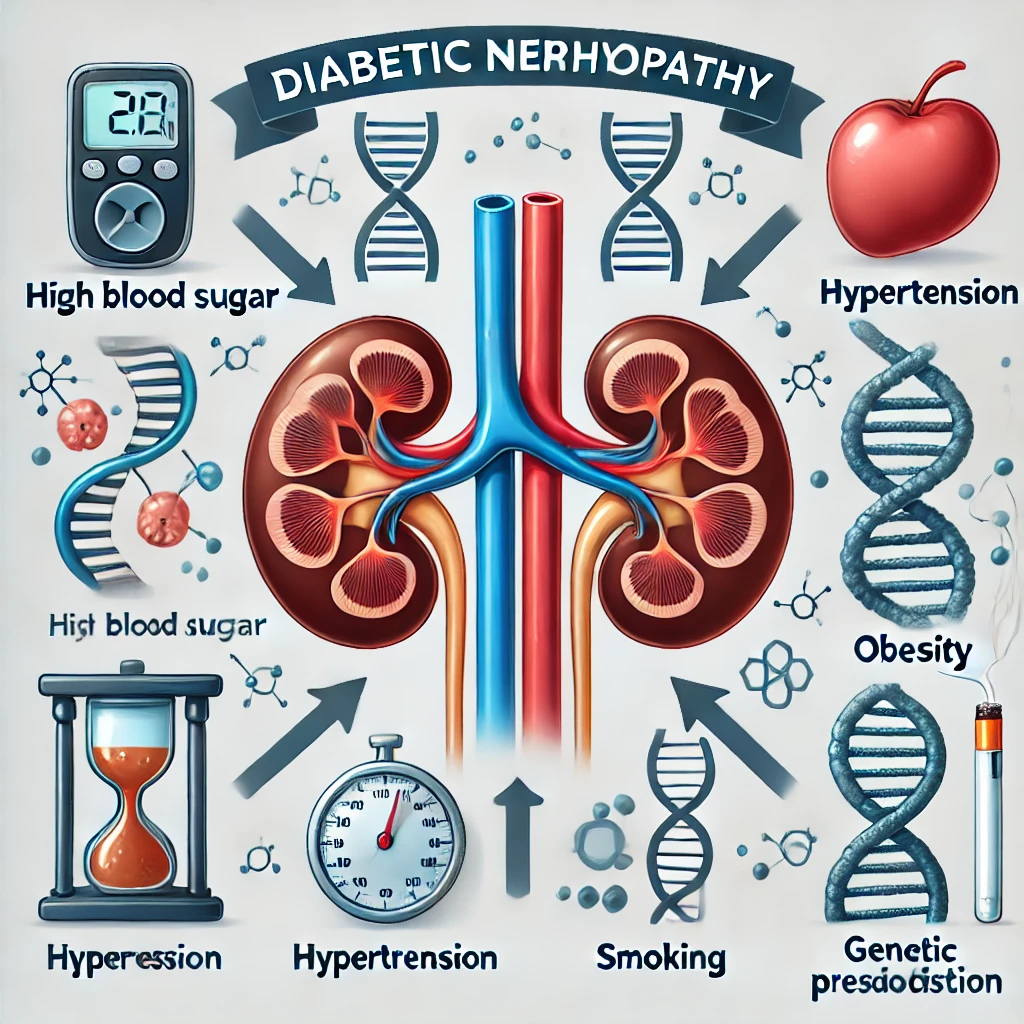
High blood pressure, which is common among individuals with diabetes, worsens kidney damage. It raises the pressure within the small blood vessels, causing extra strain and scarring. This harmful cycle of diabetes and hypertension speeds up the progression of kidney disease.
2). Genetic Predisposition and Lifestyle Influences
While diabetes and high blood pressure are key contributors to diabetic nephropathy, genetics and lifestyle choices also significantly impact the risk.
Genetic Factors:
Some people have a genetic tendency that makes them more susceptible to kidney damage. A family history of diabetes or kidney disease heightens the likelihood of developing diabetic nephropathy.
Lifestyle Choices:
Inactive lifestyles, unhealthy eating habits, and insufficient physical activity contribute to both diabetes and hypertension, increasing the risk of kidney disease.
Adopting a balanced lifestyle can greatly lower this risk by enhancing blood sugar and blood pressure management.
3). Additional Risk Factors
There are several factors, both modifiable and non-modifiable, that can affect the likelihood of developing diabetic nephropathy:
Obesity:
Carrying excess weight raises the chances of developing type 2 diabetes and high blood pressure, which can directly lead to kidney damage.
Smoking:
Smoking can speed up the progression of kidney disease by limiting blood flow to the kidneys, increasing oxidative stress, and exacerbating inflammation.
Poor Diabetes Management:
Failing to monitor blood sugar levels consistently, skipping medications, or not attending regular check-ups can result in uncontrolled diabetes, which raises the risk of nephropathy.
Duration of Diabetes:
The longer a person has diabetes, the higher the risk of experiencing kidney damage.
Age and Ethnicity:
Age and EthnicityOlder individuals and specific ethnic groups, including African Americans, Hispanics, and Native Americans, face a greater risk of diabetic nephropathy due to a combination of genetic and socioeconomic factors.
Recognizing the Symptoms of Diabetic Nephropathy
Diabetic nephropathy, also known as diabetic kidney disease, is a progressive condition that often develops quietly in people with diabetes. In the early stages, there may be no clear symptoms, but kidney damage can continue to build over time. Identifying the signs of diabetic nephropathy is essential for early intervention, which can help slow its progression and safeguard kidney function.
1). Early Symptoms: Silent Damage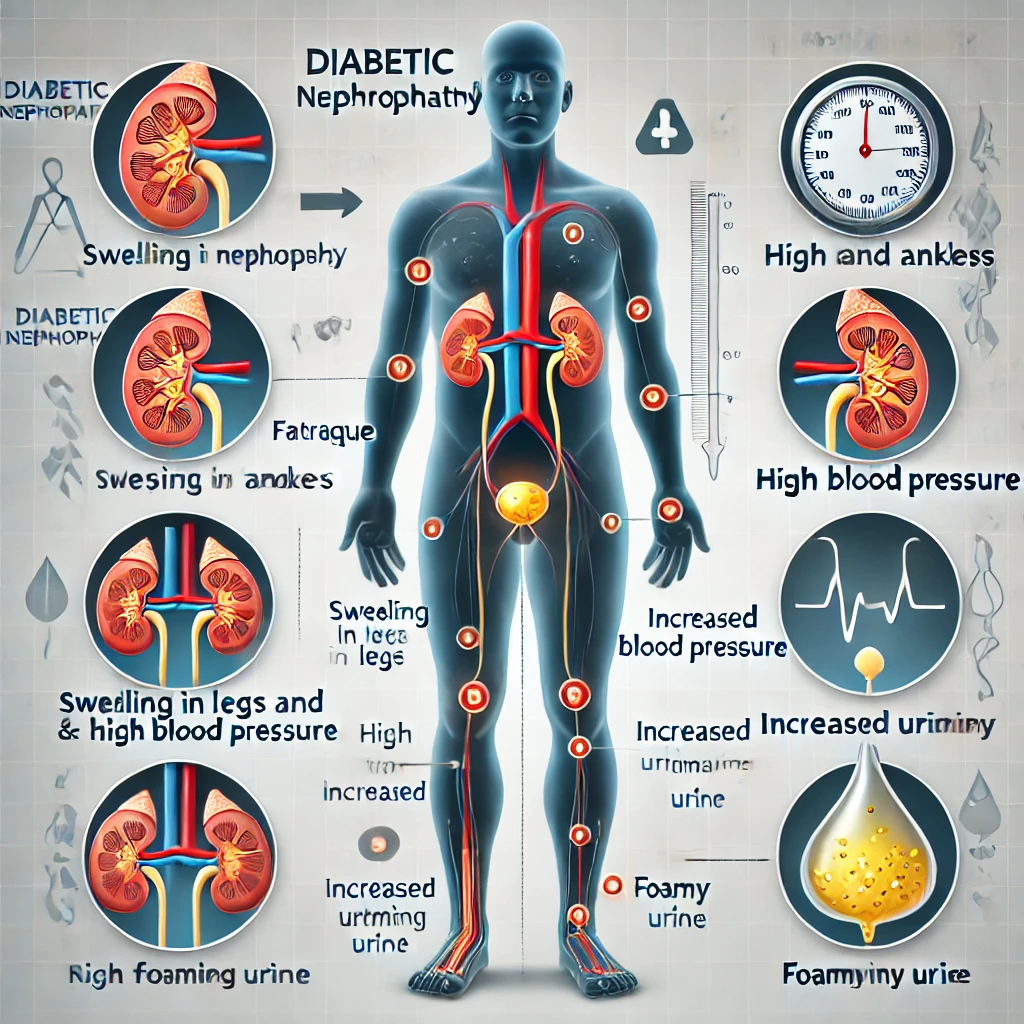
In the initial phases of diabetic nephropathy, symptoms are frequently subtle or nonexistent. However, the following indicators may suggest the early onset of kidney damage:
Foamy Urine:
The presence of protein in the urine, referred to as albuminuria, can make the urine appear foamy or bubbly. This is often one of the first noticeable signs of kidney damage.
Swelling (Edema):
Fluid retention due to compromised kidney function may lead to swelling, particularly in the feet, ankles, hands, or around the eyes.
High Blood Pressure:
While hypertension can contribute to diabetic nephropathy, it can also worsen as kidney function deteriorates, creating a harmful cycle.
2). Symptoms in Advanced Stages
As diabetic nephropathy advances, kidney damage becomes more evident, and symptoms become more pronounced:
Fatigue and Weakness:
Diminished kidney function can result in a buildup of toxins and waste products in the bloodstream, leading to fatigue, weakness, and trouble concentrating.
Nausea and Vomiting:
The accumulation of waste in the blood (uremia) can cause gastrointestinal issues such as nausea, vomiting, and a loss of appetite.
Shortness of Breath:
Fluid retention in the body, especially in the lungs, can lead to breathing difficulties.
Persistent Itching:
Elevated levels of waste products in the blood can result in skin irritation and ongoing itching.
Changes in Urination:
– Increased frequency of urination, particularly at night (nocturia).
– Dark, cloudy, or bloody urine in severe cases.
– Decreased urine output as kidney function declines
When to Seek Medical Attention
Many symptoms of diabetic nephropathy can be similar to those of other health issues, making it crucial for people with diabetes to have regular medical check-ups. You should reach out for medical help if you experience:
Ongoing swelling in your legs, feet, or face.
Notable changes in how often you urinate.
Feelings of fatigue, nausea, or unexpected weight loss.
High blood pressure that becomes hard to control.
Importance of Regular Screening
Since diabetic nephropathy can develop without clear symptoms, regular kidney function tests are essential for early detection:
Urine Tests: To check for protein (albumin) in the urine.
Blood Tests: To assess creatinine levels and estimate the glomerular filtration rate (GFR), which reflects kidney function.
Blood Pressure Monitoring: High blood pressure is often linked to declining kidney function.
Conclusion
The early signs of diabetic nephropathy can easily go unnoticed, which is why proactive screening is so important for those with diabetes. If detected early, kidney damage can be slowed or even prevented through effective management of blood sugar and blood pressure, along with lifestyle adjustments and medical treatments. By remaining alert and informed, individuals with diabetes can take control of their kidney health and steer clear of the serious complications associated with advanced diabetic nephropathy.